Daibetic Retinopathy
What is Daibetic Retinopathy?
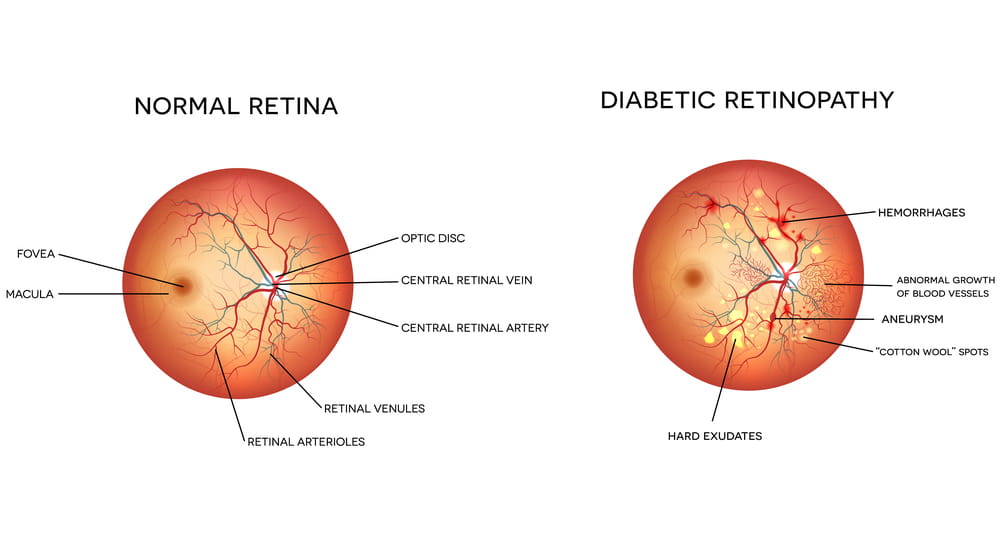
Diabetic retinopathy (DR) is the most common type of diabetic eye disease and the leading cause of blindness. Diabetes causes damage to the blood vessels of the retina, a thin and delicate tissue that is responsible for vision. In some people suffering from DR, blood vessels swell and leak fluid. In others, abnormal new blood vessels grow on the surface of the retina that can lead to bleeding and retinal detachment. A healthy retina is necessary for good vision.
If you have diabetic retinopathy, at first you may not notice changes to your vision. Yet over time, the condition can worsen and cause vision loss. Diabetic retinopathy usually affects both eyes, but early detection and prompt treatment can minimize vision loss.
Stages Of Diabetic Retinopathy:
MODERATE NONPROLIFERATIVE RETINOPATHY
Moderate nonproliferative retinopathy is essentially a progression from the mild stage. Many more microaneurysms, hemorrhages and cotton wool spots emerge and there is further damage to the retinal blood vessels. The danger is that such damage can result in reduced blood flow to the surrounding retinal tissue leading to vision loss.
MILD NONPROLIFERATIVE RETINOPATHY
The features of mild nonproliferative retinopathy are some of the earlier stages of diabetic retinopathy. At this point, small areas of balloon-like dilation of blood vessels, called microaneurysms, start to appear along with other findings such as small spot hemorrhages and cotton wool spots. It's important to note that not all patients with mild nonproliferative retinopathy will notice a change in their vision.
SEVERE NONPROLIFERATIVE RETINOPATHY
As the retinopathy progresses and more blood vessels have now been affected, larger areas of the retina are deprived of blood flow, these are known as capillary non perfusion areas. This results in the retina producing new blood vessels in an attempt to enhance nourishment.
PROLIFERATIVE RETINOPATHY
At this advanced stage, the signals sent by the retina for nourishment trigger the growth of new blood vessels that grow along the retina and into other parts of the eye. These blood vessels are abnormal and fragile, often leading to the development of new or worsening existing symptoms and frequent vision loss. Left untreated, severe vision loss and even permanent blindness can result.
How does diabetic retinopathy cause vision loss?
Damaged blood vessels from diabetic retinopathy can cause vision loss in several ways:
Fluid can leak into the macula, the center of the retina that is responsible for central vision. Just like a damaged garden hose, the damaged blood vessels surrounding the macula leak, and fluid accumulates around the surrounding macular tissue, causing it to swell and creating blurry vision. This is called diabetic macular edema(DME) and it can occur at any stage of diabetic retinopathy. It is the most common cause for reduced vision in diabetics.
Abnormal new blood vessels can grow from the damaged retina. These fragile vessels tend to break and produce bleeding along the retina and vitreous cavity. This is called a vitreous hemorrhage and commonly causes floaters and, in severe cases, leads to vision loss. If left untreated at this stage it can further deteriorate into Tractional Retinal Detachment (TRD).
Who is at risk for diabetic retinopathy?
All diabetics—both Types 1 & 2—are at risk, which is why everyone with diabetes should get a comprehensive dilated eye exam at least once a year. The longer someone has diabetes, the more likely he or she will develop diabetic retinopathy. It's fortunate that in most cases diabetic retinopathy is a treatable condition.
Diabetic retinopathy may be a problem for women with diabetes during pregnancy. To protect vision, every pregnant woman with diabetes should have a comprehensive dilated eye exam as early as possible.
What can I do to protect my vision?
DILATED EYE EXAMS
Early detection and treatment can prevent vision loss. If you are diabetic, be sure to schedule a comprehensive dilated eye exam at least twice a year. It is important to remember that your diabetic retinopathy can progress without symptoms. You can develop both proliferative retinopathy and macular edema and still see normally, but you may remain at high risk for vision loss. A retina specialist can tell if you have any stage of diabetic retinopathy or macular edema. Depending on the severity of your diabetic retinopathy, your doctor may suggest you have more frequent exams.
BLOOD SUGAR CONTROL
Better control of blood sugar levels slows the onset and progression of retinopathy. In general, diabetic patients who kept their blood sugar levels as close to normal as possible also had significantly less kidney and nerve disease. Better control also reduced the need for sight-saving treatment. Patients should routinely see their primary care provider who can determine the best form of blood sugar control for you. Control of associated Hypertension and blood cholesterol is also advised for optimal result.
How will I know if I have diabetic retinopathy?
EARLY SYMPTOMS
There are often no symptoms during the early stages of the disease, nor is there any pain. It's important, therefore, not to wait for symptoms. When symptoms do occur, they range from mildly blurred central vision to complete vision loss. It specifically causes problems in reading and near vision. It is critical to secure prompt medical attention if you notice any change in your vision.
SYMPTOMS OF ADVANCED DISEASE
Proliferative retinopathy frequently produces symptoms as a result of bleeding into the vitreous cavity. At first, you may notice a few specks of blood "floating" in your vision. If that occurs, see your retina specialist as soon as possible; you may need treatment before more serious bleeding occurs. Hemorrhages tend to happen more than once, often during sleep. Sometimes, even without treatment, the spots are clear, and your vision will improve. Yet it's more likely that bleeding will reoccur and cause severely blurred vision. You need to be examined by your retina specialist at the first sign of blurred vision, before more bleeding occurs. The earlier you receive treatment, the more likely treatment will be effective. If left untreated, proliferative retinopathy can cause severe vision loss and even blindness.
How is diabetic retinopathy diagnosed?
Diabetic retinopathy is detected during a comprehensive eye exam. After checking your vision and eye pressure, drops are placed in your eyes to widen, or dilate, the pupils. A retina specialist uses a special magnifying lens to examine your retina for signs of diabetic retinopathy.
Your retina specialist may also order special testing to help stage the retinopathy or decide if treatment is needed. One test, a fluorescein angiogram, uses a special dye that is injected into your arm. Pictures are taken as the dye passes through the blood vessels in your retina, allowing for the identification of any leaking blood vessels that may require treatment. Your doctor may also recommend Ocular Coherence Tomography, or OCT, to check for diabetic macular edema. This is a non-invasive test, similar to an ultrasound or CT scan, that helps detect fluid within the macula. After the exam, your close-up vision may remain blurred for several hours due to the dilating drops.
How is a diabetic macular edema treated?
FOCAL/ GRID LASER TREATMENT
Macular edema is most effectively treated with focal laser treatment that is usually completed in one session. Your doctor seals leaking blood vessels (microaneurysms) with light heat generated by a laser. These treatment spots slow the leakage of fluid and reduce the amount of fluid in the macula. Focal laser treatment slows the rate of vision loss by about 50 percent and can improve visual acuity. You may need focal laser more than once to control the leaking fluid. For more wide-spread macular swelling (edema), grid laser is often used.
What happens during laser treatment?
Both focal and grid laser treatments are performed in your doctor's office with the lights dimmed. Before the treatment, your physician will dilate your pupil and apply drops to numb the eye. As you sit facing the laser machine, your doctor will hold a special lens to your eye. During the procedure, you will see flashes of bright light. Although the flashing lights are often described as annoying, there is generally little to no discomfort associated with this procedure.
Laser treatment will at best stabilize vision, but generally cannot restore vision that has been lost. This is yet another reason that treating diabetic retinopathy early is the best way to prevent vision loss.
INTRAVITREAL INJECTIONS
Certain drugs have been used to successfully reduce macular edema and new blood growth resulting from diabetic retinopathy
ANTI-VEGF INJECTION THERAPY
Anti-VEGF drugs are injected into the vitreous gel to block a protein called vascular endothelial growth factor (VEGF), which can stimulate abnormal blood vessels to grow and leak fluid. Blocking VEGF can reverse abnormal blood vessel growth and decrease fluid in the retina. Available anti-VEGF drugs include Avastin (bevacizumab), Lucentis (ranibizumab), and Eylea (aflibercept). Lucentis and Eylea are approved by the U.S. Food and Drug Administration (FDA) for treating DME. Avastin was approved by the FDA to treat cancer, but is commonly used to treat eye conditions, including DME.
Most people require monthly anti-VEGF injections for the first 3-6 months of treatment. Thereafter, injections are needed less often.
CORTICOSTEROIDS
Corticosteroids, either injected or implanted into the eye, may be used alone or in combination with other drugs or laser surgery to treat DME. The Ozurdex (dexamethasone) implant is for 6 months duration, while Triamcinolone (tricort) is for 2 months duration. Corticosteroid use in the eye increases the risk of cataract and glaucoma (much more with tricort than Ozurdex).
How is proliferative diabetic retinopathy treated?
There are two major therapies for proliferative diabetic retinopathy—Pan retinal photocoagulation laser treatment and vitrectomy.
PANRETINAL PHOTOCOAGULATION
Scatter laser treatment helps to shrink the abnormal blood vessels. Your doctor places laser spots throughout the entire peripheral retina, causing the abnormal blood vessels to shrink. Because it's necessary to use a large number of laser spots, more than one session (3-4) is often required to complete treatment. Scatter laser treatment is needed to preserve your central vision. This treatment is more effective before the fragile, new blood vessels have started to bleed, even if bleeding has begun, scatter laser treatment may still be possible, based on the amount of bleeding
In some instances, anti-VEGF drugs may be used in conjunction with laser to treat severe forms of proliferative diabetic retinopathy.
Some degree of discomfort is common with this treatment. It usually subsides at the end of the procedure, but some patients report mild discomfort or a mild headache lasting for the rest of the day. Other complications are rare, but will be explained prior to your procedure.
VITRECTOMY
You may require a surgical procedure called a vitrectomy if bleeding is severe, if it does not clear up on its own or if you develop a retinal detachment related to your diabetic retinopathy. This procedure is almost always performed under local anesthesia. Your doctor inserts tiny instruments through small incisions in the sclera (the white portion of the eye) and removes the gel and blood from the center of the eyeball. He or she will then replace the clouded gel with a clear saline solution or gas bubble or silicone oil. Following the procedure, an eye patch is placed on the operated eye and you need to return to the office the next day.
Are scatter laser treatment and vitrectomy effective in treating proliferative retinopathy?
Both are very effective in reducing vision loss. Although they both have high success rates, neither one cures diabetic retinopathy, but rather reduces the risk of new bleeding. Vitrectomy surgery can—and usually does—improve vision, but scatter lasers are employed to stabilize vision. You may need multiple treatments to protect your sight.